| PREFACE |
To the Readers, embarking on the creation of “How to Be a Good Nurse” has been both a privilege and a passion. This book is born from the belief that nursing is not just a profession but a profound journey of compassion, skill, and continuous growth. In these pages, you will find more than information; you will discover a reservoir of insights, anecdotes, and practical wisdom garnered from the diverse tapestry of the nursing world. As a nurse, educator, and lifelong learner, my goal is to offer you a compass in your own journey whether you are a novice navigating the early stages of your career or a seasoned professional seeking to enrich your practice. This book is not a prescription but a conversation, a dialogue that invites you to reflect, learn, and evolve. Each chapter is crafted with care, addressing the multifaceted aspects of nursing from foundational skills to the intricacies of ethical decision-making, from the art of communication to the challenges of leadership. Consider this book as a companion, accompanying you through the highs and lows, the triumphs and tribulations inherent in the noble path of nursing. Thank you for entrusting me with a small part of your learning journey. May “How to Be a Good Nurse” inspire you, challenge you, and above all, empower you to be the exceptional nurse you aspire to become. With heartfelt dedication,
[Nr. Ahmad Adam R.N]
| CHAPTER ONEFOUNDATION OF NURSING PRACTICE |
INTRODUCTION
In the heart of healthcare lies a profession that blends science with humanity, and that is the essence of nursing. “How to Be a Good Nurse” is not a mere manual but a compass guiding you through the labyrinth of nursing, helping you unlock the secrets to being not just a good nurse but an exceptional one. As you flip through these pages, envision a journey that transcends textbooks and enters the pulse of real-life patient care. This book is a tapestry woven with the threads of empathy, expertise, and unwavering commitment a guide for those who seek not just a career but a calling. From mastering clinical skills to navigating the complex web of ethical decisions, we embark on a quest to equip you with the armor of knowledge and the wings of compassion. Whether you’re a novice nurse stepping into the world of healthcare or a seasoned professional looking to refine your craft, this book is a roadmap to excellence. Join me as we explore the art and science of nursing a journey that transforms the ordinary into the extraordinary, the routine into the remarkable. “How to Be a Good Nurse” is more than a book; it’s an invitation to embrace the challenges, celebrate the victories, and, above all, embrace the profound impact you can make in the lives of those entrusted to your care.
Ethics in Nursing
Ethics in nursing refers to the moral principles and standards that guide the behavior and decisions of nurses in their professional practice. It involves a set of principles that govern the nurse’s conduct, emphasizing values such as honesty, integrity, and respect for the dignity and rights of patients. Ethical considerations in nursing include respecting patient autonomy, maintaining confidentiality, and making decisions that prioritize the well-being of the patient.
Values in Nursing
Values in nursing encompass the core beliefs and principles that shape a nurse’s attitudes and actions. These values influence how nurses interact with patients, families, colleagues, and the broader healthcare community. Common nursing values include compassion, empathy, altruism, integrity, and a commitment to providing high-quality patient care. Values in nursing serve as a foundation for ethical decision-making and guide nurses in delivering patient-centered and culturally sensitive care.
The significance of ethics and values in healthcare is profound, influencing various aspects of patient care, professional conduct, and the overall functioning of the healthcare system. Here are some key reasons why ethics and values play a crucial role in healthcare:
1. Patient-Centered Care:
Ethics and values guide healthcare professionals to prioritize the well-being and autonomy of patients. This ensures that patient care is focused on meeting individual needs and preferences.
2. Trust and Professionalism:
Adherence to ethical standards builds trust between healthcare providers, patients, and the community. Professionalism, rooted in ethical conduct, enhances the credibility and reputation of healthcare professionals and institutions
3. Informed Decision-Making:
Ethical principles, such as autonomy and informed consent, empower patients to actively participate in their healthcare decisions. This fosters a collaborative approach between healthcare providers and patients
4. Patient Advocacy:
Ethical nurses and healthcare professionals act as advocates for their patients, ensuring their rights are respected and their best interests are represented in the healthcare decision-making process
5. Quality of Care:
Ethical conduct contributes to the delivery of high-quality healthcare. Following ethical guidelines ensures that healthcare professionals provide evidence-based, effective, and safe care, contributing to positive patient outcomes.
6. Equity and Fairness: Ethical considerations address issues of fairness and equity in healthcare delivery. Ensuring equal access to healthcare services and avoiding discrimination are fundamental ethical principles.
7. Team Collaboration:
Shared ethical values foster collaboration among healthcare team members. This enhances communication, coordination, and mutual respect among professionals from different disciplines, ultimately benefiting patient care.
8. Legal Compliance:
Adherence to ethical standards often aligns with legal requirements. Healthcare professionals and institutions that uphold ethical principles are more likely to comply with legal regulations, reducing the risk of legal issues.
9. Public Perception and Reputation:
Healthcare organizations and professionals with a strong commitment to ethics and values are viewed positively by the public. This positive perception contributes to a good reputation and can attract patients and support from the community.
10. Prevention of Exploitation and Abuse:
Ethical guidelines serve as a safeguard against potential abuse or exploitation of vulnerable populations. They establish boundaries and standards to protect patients from harm.
11. Continuous Improvement:
Ethical reflection and adherence to values encourage a culture of continuous improvement in healthcare. Professionals engage in ongoing education and self-assessment to stay updated on ethical considerations and best practices.
In summary, ethics and values are foundational to the ethical practice of healthcare, ensuring that patient care is compassionate, respectful, and aligned with the principles of justice and beneficence. They contribute to a healthcare environment that prioritizes the needs and well-being of patients while fostering professionalism and trust among healthcare providers.
LEGAL ASPECT OF NURSING
The legal aspects of nursing encompass a range of regulations and laws that govern the practice of nursing to ensure patient safety, quality care, and ethical standards. Here are key legal aspects relevant to nursing:
1. Licensure and Certification:
Nurses must obtain and maintain a valid nursing license to practice legally. Licensing requirements vary by jurisdiction, and nurses must adhere to the regulations set by nursing boards or regulatory bodies.
2. Scope of Practice:
Each nurse must work within their defined scope of practice, which outlines the specific activities and responsibilities they are authorized to perform. Deviating from the scope of practice may lead to legal consequences.
3. Documentation and Record-Keeping:
Accurate and timely documentation of patient care is a legal requirement. Nurses must maintain detailed records of assessments, interventions, and patient outcomes, as these documents are essential for communication, continuity of care, and legal protection.
4. Informed Consent:
Nurses play a role in obtaining informed consent from patients before medical procedures or treatments. Understanding and respecting the legal principles of informed consent is crucial to avoid legal issues related to patient autonomy.
5. Confidentiality and HIPAA Compliance:
Nurses are obligated to maintain patient confidentiality and comply with the Health Insurance Portability and Accountability Act (HIPAA). Unauthorized disclosure of patient information can lead to legal consequences.
6. Mandatory Reporting:
Nurses are mandated reporters, required to report instances of abuse, neglect, or certain communicable diseases. Failure to report as mandated by law can result in legal consequences.
7. Patient Rights:
Nurses must be aware of and respect patients’ rights, including the right to privacy, dignity, and access to quality care. Violation of patient rights may lead to legal actions.8.Professional Liability (Malpractice):
Nurses can be held legally accountable for professional negligence or malpractice. Malpractice claims may arise if a nurse fails to meet the standard of care, leading to harm or injury to the patient.
9. Whistleblower Protection:
Nurses who report unlawful or unsafe practices within their workplace, known as whistleblowers, are protected by law from retaliation. Reporting concerns about patient safety is considered an ethical and legal obligation.
10. Workplace Safety:
Nurses have the right to work in a safe environment. Employers are legally obligated to provide a safe workplace, including measures to prevent workplace violence and exposure to hazardous materials.
11. Continuing Education and Competency:
Legal requirements often mandate that nurses engage in ongoing education to maintain and update their professional competence. Failure to meet these requirements may affect licensure and legal standing.
12. Advance Directives and End-of-Life Care:
Nurses must understand and respect legal documents such as advance directives and living wills. Compliance with legal requirements for end-of-life care, including do-not-resuscitate (DNR) orders, is essential.
Staying informed about these legal aspects is crucial for nurses to practice ethically, protect themselves legally, and provide safe and effective patient care. It’s important to note that legal requirements may vary by jurisdiction, so nurses should be familiar with the specific laws and regulations applicable in their practice area.
PROFESSIONAL CODES OF ETHICS
Professional codes of ethics serve as guiding principles for individuals within a specific profession, outlining expected standards of conduct, professional responsibilities, and ethical behavior. In the context of nursing, there are prominent codes of ethics that nurses adhere to. Here are two significant examples:
American Nurses Association (ANA) Code of Ethics for Nurses:
The ANA Code of Ethics for Nurses is a foundational document that provides guidance for ethical nursing practice. It consists of nine provisions, each addressing a specific aspect of ethical behavior in nursing. Some key principles include:
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
International Council of Nurses (ICN) Code of Ethics for Nurses:
The ICN Code of Ethics is a global framework that sets forth the ethical standards for nurses worldwide. It emphasizes the nurse’s commitment to promoting health, preventing illness, and advocating for the rights of patients. Key principles include:
Principle 1: Nurses and nursing care have human rights and the rights of people to receive information, participate in decision-making, and receive competent care based on ethical standards.
Principle 4: Nurses have the responsibility to maintain the highest standards of health care and provide services with respect for human dignity and cultural differences. These codes of ethics share common themes such as respect for human dignity, advocacy for patient rights, maintaining confidentiality, and providing competent and compassionate care. Nurses are expected to integrate these ethical principles into their daily practice, fostering a commitment to professionalism and patient-centered care.
It’s essential for nurses to familiarize themselves with the specific code of ethics relevant to their region or professional organization. Adhering to these codes not only ensures ethical nursing practice but also contributes to building trust with patients, colleagues, and the broader healthcare community.
The exploration of nursing codes of ethics involves a deeper understanding of the principles and provisions that guide ethical nursing practice. Let’s delve into some key aspects of the American Nurses Association (ANA) Code of Ethics for Nurses, as it is a widely recognized and influential code in the field:
Overview of ANA Code of Ethics for Nurses:
Provision 1: The Nurse Practices with Compassion and Respect for the Inherent Dignity, Worth, and Unique Attributes of Every Person.
Implications:
- Nurses are called to recognize and respect the individuality of each patient.
- Emphasis on providing care that is considerate and understanding of the patient’s values, beliefs, and cultural background.
Provision 3: The Nurse Promotes, advocates for, and Protects the Rights, Health, and Safety of the Patient.
Implications:
- Nurses are advocates for patients, ensuring their rights are upheld.
- Responsibility to create a safe and healthy environment for patients, addressing potential risks and advocating for necessary resources.
Provision 4: The Nurse Has Authority, Accountability, and Responsibility for Nursing Practice.
Implications:
- Nurses have a duty to maintain competence and continually enhance their professional skills.
- Accountability for their nursing practice, including delegation of tasks and collaboration within the healthcare team.
Provision 5: The Nurse Owes the Same Duties to Self as to Others, Including the Responsibility to Preserve Integrity and Safety, to Maintain Competence, and to Continue Personal and Professional Growth.
Implications:
- Nurses are encouraged to prioritize their own well-being to provide effective care.
- Continuous self-reflection, professional development, and maintaining personal and professional boundaries.
Provision 8: The Nurse Collaborates with Other Health Professionals and the Public in Promoting Community, National, and International Efforts to Meet Health Needs.
Implications:
- Emphasis on interdisciplinary collaboration for the benefit of patient care
- Involvement in community health initiatives and advocating for healthcare policies that address public health needs.
Provision 9: The Profession of Nursing, as Represented by Associations and their Members, is Responsible for Articulating Nursing Values, for Maintaining the Integrity of the Profession and its Practice, and for Shaping Social Policy.
Implications:
- Nurses and nursing associations play a role in shaping the profession and influencing policies.
- Advocacy for nursing values and the overall integrity of the profession.
Conclusion: The ANA Code of Ethics for Nurses provides a comprehensive framework that encourages nurses to integrate ethical considerations into their practice. It emphasizes the importance of patient-centered care, professional responsibility, self-care, collaboration, and advocacy. This exploration serves as a guide for nurses to navigate ethical dilemmas and contribute to the advancement of the nursing profession.
Understanding and adhering to professional standards is crucial for nurses to ensure high-quality patient care, maintain ethical conduct, and contribute to the overall integrity of the nursing profession. Here are some key aspects of understanding and adding to professional standards in nursing:
Understanding Professional Standards:
Code of Ethics:
Familiarize yourself with the nursing code of ethics relevant to your region or professional organization (e.g., ANA Code of Ethics). Understand the principles and provisions that guide ethical nursing practice.
Scope of Practice:
Clearly understand your defined scope of practice, which outlines the activities and responsibilities you are authorized to perform. Adhering to this scope ensures safe and legal nursing practice.
Licensing Requirements:
Stay informed about the licensing requirements in your jurisdiction. Ensure that your nursing license is current and that you meet any continuing education or renewal requirements.
Professional Organizations:
Engage with professional nursing organizations (e.g., American Nurses Association, International Council of Nurses) to stay updated on industry standards, best practices, and emerging trends.
Clinical Guidelines and Protocols:
Adhere to evidence-based clinical guidelines and protocols relevant to your specialty. Stay informed about updates and revisions to ensure current and effective practice.
Quality Improvement:
Participate in quality improvement initiatives within your healthcare setting. Contribute to efforts that enhance patient outcomes, safety, and overall quality of care.
Adding to Professional Standards:
Continuing Education:
Pursue continuous professional development through ongoing education. Attend workshops, conferences, and training sessions to stay updated on new technologies, treatments, and best practices.
Research and Evidence-Based Practice:
Contribute to the advancement of nursing knowledge by staying informed about current research. Consider engaging in research projects or incorporating evidence-based practices into your clinical setting.
Mentorship and Leadership:
Serve as a mentor to less experienced colleagues and contribute to the professional development of others. Consider taking on leadership roles that allow you to influence and shape nursing practice within your organization.
Advocacy and Policy Involvement:
Advocate for policies and practices that promote patient rights, safety, and improved healthcare outcomes. Get involved in discussions and initiatives that impact the nursing profession at a broader level.
Interdisciplinary Collaboration:
Foster collaboration with other healthcare professionals to promote a multidisciplinary approach to patient care. Contribute to effective communication and teamwork within the healthcare team.
Self-Reflection and Professionalism:
Engage in regular self-reflection to assess your own professional growth and areas for improvement. Uphold the highest standards of professionalism, ethics, and integrity in your interactions with patients, colleagues, and the community.
By actively understanding and contributing to professional standards, nurses play a pivotal role in maintaining the integrity of the nursing profession and ensuring that patient care is of the highest quality. Continuous learning, advocacy, and leadership contribute to the ongoing advancement of nursing practice and standards.
| CHAPTER TWOCLINICAL SKILLS AND TECHNIQUES |
CLINICAL SKILLS AND TECHNIQUES
Clinical skills and techniques are essential for nurses to provide safe, effective, and patient-centered care. Here’s an overview of some key clinical skills and techniques that nurses commonly utilize in various healthcare settings:
1. Patient Assessment:
Technique: Conduct thorough physical assessments, including vital signs, neurological assessments, and focused assessments based on the patient’s condition.
Skill: Ability to systematically and accurately assess a patient’s health status, identifying potential issues or changes.
2. Medication Administration:
Technique: Administering medications via various routes, ensuring accurate dosage and adhering to safety protocols.
Skill: Proficiency in calculating dosages, understanding medication interactions, and maintaining meticulous documentation.
3. Intravenous (IV) Therapy:
Technique: Inserting and managing intravenous lines, administering fluids and medications intravenously.
Skill: Competence in venipuncture, selecting appropriate IV sites, and preventing complications related to IV therapy.
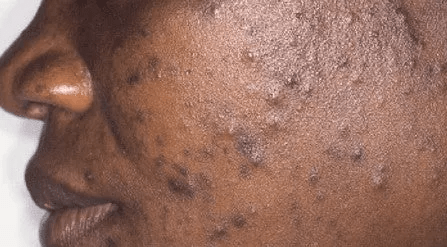
4. Wound Care:
Technique: Assessing and dressing wounds, preventing infections, and promoting optimal wound healing.
Skill: Understanding wound types, using aseptic techniques, and selecting appropriate dressings based on the wound’s characteristics.
5. Patient Positioning and Mobility:
Technique: Safely assisting patients with positioning, transferring, and mobilizing.
Skill: Preventing patient injuries, maintaining proper body mechanics, and addressing the individualized mobility needs of patients.
6. Nursing Procedures:
Technique: Performing various nursing procedures such as urinary catheterization, NG tube insertion, and tracheostomy care.
Skill: Following evidence-based protocols, ensuring patient comfort, and minimizing the risk of complications.
7. Cardiopulmonary Resuscitation (CPR):
Technique: Administering CPR in emergency situations to restore cardiac and respiratory function.
Skill: Mastery of chest compressions, airway management, and defibrillator use to respond effectively to cardiac arrest.
8. Physical Examination:
Technique: Conducting systematic head-to-toe physical examinations to assess overall patient health.
Skill: Competence in performing focused examinations based on patient complaints or specific health conditions.
9. Communication Skills:
Technique: Effective communication with patients, families, and healthcare team members.
Skill: Active listening, empathy, and clear communication to establish rapport, provide information, and address patient concerns.
10. Electronic Health Record (EHR) Use:
Technique: Navigating and documenting patient information in electronic health record systems.
Skill: Ensuring accurate and timely documentation, maintaining patient confidentiality, and utilizing technology for efficient care delivery.
11. Pain Management:
Technique: Assessing and managing pain using various interventions and medications.
Skill: Tailoring pain management plans to individual patient needs, evaluating effectiveness, and addressing potential side effects.
12. Infection Control:
Technique: Implementing infection prevention measures, including hand hygiene, isolation precautions, and proper use of personal protective equipment (PPE).
Skill: Minimizing the risk of healthcare-associated infections and promoting a safe environment.
Conclusion: Nurses continually enhance and update their clinical skills and techniques through ongoing education, training, and practical experience. The mastery of these skills is integral to delivering high-quality, patient-centered care in diverse healthcare settings.
| CHAPTER THREECOMMUNICATION SKILLS |
COMMUNICATION SKILLS
Communication skills are fundamental for nurses to establish rapport with patients, collaborate with the healthcare team, and ensure effective care delivery. Here are key aspects of communication skills for nurses:
1. Therapeutic Communication:
Definition: Therapeutic communication is a dynamic and purposeful interaction between the nurse and the patient that promotes a positive and healing relationship.
Skills:
- Active Listening: Giving full attention, providing feedback, and demonstrating understanding.
- Empathy: Understanding and sharing the feelings of the patient.
- Open-ended Questions: Encouraging patients to express themselves in their own words.
2. Patient and Family Education:
Definition: Effectively conveying health information to patients and their families to empower them in making informed decisions.
Skills:
- Clear Explanation: Using simple language, avoiding jargon, and ensuring patient comprehension.
- Encouraging Questions: Creating an environment where patients feel comfortable asking questions.
- Use of Visual Aids: Utilizing visual materials to enhance understanding.
3. Interdisciplinary Communication:
Definition: Collaborating and communicating with members of the healthcare team to ensure comprehensive patient care.
Skills:
- Effective Handoff: Providing accurate and concise information during shift changes.
- Team Meetings: Actively participating in team discussions and sharing relevant patient information.
- Conflict Resolution: Addressing conflicts professionally and finding solutions collaboratively.
4. Nonverbal Communication:
Definition: Conveying messages without using words, including facial expressions, body language, and gestures.
Skills:
- Eye Contact: Establishing and maintaining appropriate eye contact to convey attentiveness.
- Body Language: Using open and welcoming gestures to enhance communication.
- Facial Expressions: Displaying empathy and understanding through facial cues.
5. Cultural Competence:
Definition: Recognizing and respecting diverse cultural backgrounds and effectively communicating across cultural differences.
Skills:
- Cultural Awareness: Being aware of one’s own cultural biases and beliefs.
- Language Competency: Utilizing interpreters when needed and respecting linguistic diversity.
- Cultural Sensitivity: Adapting communication styles to meet the cultural needs of patients.
6. Confidentiality and Privacy:
Definition: Respecting and protecting patient privacy by maintaining confidentiality.
Skills:
- Secure Information Sharing: Ensuring that patient information is shared only with authorized individuals.
- Closed-Door Conversations: Conducting private discussions in appropriate settings.
7. Professional Boundaries:
Definition: Maintaining appropriate professional relationships with patients and colleagues.
Skills:
- Maintaining Objectivity: Avoiding personal disclosure and keeping the focus on patient care.
- Respecting Personal Space: Being mindful of physical boundaries and personal space.
8. Empathetic Communication:
Definition: Conveying understanding and compassion to patients, acknowledging their emotions.
Skills:
- Reflective Responses: Mirroring the patient’s feelings to convey empathy.
- Validation: Recognizing and validating the patient’s emotions and experiences.
Conclusion: Communication skills are integral to the nursing profession, influencing patient outcomes, satisfaction, and the overall quality of healthcare delivery. Continuous development and refinement of these skills contribute to effective patient care and positive interactions within the healthcare team.
| CHAPTER-FOURCRITICAL THINKING AND DECISION-MAKING |
CRITICAL THINKING AND DECISION MAKING
Critical thinking and decision-making are integral skills for nurses, allowing them to assess situations, analyze information, and make informed choices that positively impact patient care. Here’s an exploration of critical thinking and decision-making in the context of nursing:
Critical Thinking:
Definition: Critical thinking is the ability to objectively analyze information, assess situations, and make reasoned judgments.
Key Components:
- Analysis: Breaking down complex information into manageable parts.
- Evaluation: Assessing the reliability and relevance of information.
- Inference: Drawing logical conclusions based on available evidence.
- Problem-solving: Developing solutions to challenges or issues.
Application in Nursing:
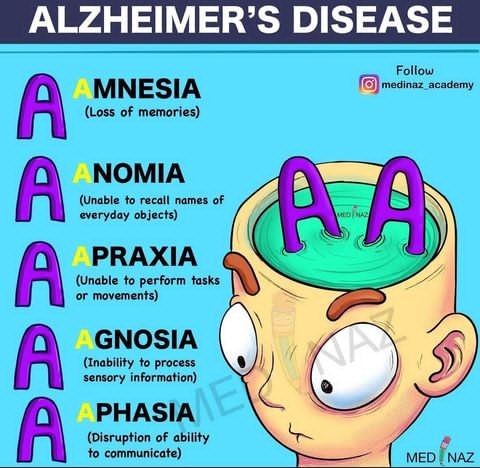
- Clinical Reasoning: Applying critical thinking to clinical situations for effective decision-making.
- Diagnostic Reasoning: Formulating accurate nursing diagnoses based on patient assessment.
Example: When faced with a patient exhibiting unusual symptoms, a nurse uses critical thinking to analyze the symptoms, consider potential causes, and determine the appropriate course of action for further assessment or intervention.
Decision-Making:
Definition: Decision-making involves choosing a course of action from several alternatives, considering potential outcomes and their consequences.
Key Components:
- Identification of Options: Recognizing possible courses of action.
- Consideration of Consequences: Evaluating potential outcomes and impacts.
- Risk Assessment: Weighing the risks and benefits associated with each option.
Application in Nursing:
- Clinical Decision-Making: Choosing the most appropriate interventions based on patient needs and evidence-based practice.
- Prioritization: Ranking nursing interventions based on the urgency and importance of patient needs.
Example: Faced with conflicting patient priorities, a nurse employs decision-making skills to prioritize interventions, considering the urgency of each task and the potential impact on patient outcomes.
Integration in Nursing Practice:
Patient Assessment: Critical thinking is essential in accurately assessing patient conditions, recognizing patterns, and identifying relevant data.
Care Planning: Nurses utilize critical thinking to develop individualized care plans based on patient needs, integrating evidence-based practices.
Communication: Effective communication with patients, families, and the healthcare team requires critical thinking to convey information clearly and gather relevant data.
Problem-Solving: Nurses engage in problem-solving to address unexpected challenges, adapting care plans as needed for optimal patient outcomes.
Continuous Development:
Education: Nurses engage in ongoing education to stay current with medical advancements, evidence-based practices, and evolving healthcare standards.
Reflection: Regular reflection on clinical experiences helps nurses identify areas for improvement and refine their critical thinking and decision-making skills.
Interdisciplinary Collaboration: Collaborating with other healthcare professionals enhances critical thinking by incorporating diverse perspectives in decision-making processes.
Conclusion: Critical thinking and decision-making are dynamic processes that are central to nursing practice. Developing and honing these skills contribute to the provision of high-quality,
patient-centered care and the continuous improvement of nursing practice.
| CHAPTER-FIVEPROFESSIONAL DEVELOPMENT |
PROFESSIONAL DEVELOPMENT
Professional development in nursing is a lifelong, intentional process of acquiring knowledge, skills, and experiences to enhance one’s abilities and advance within the nursing profession. Here are key aspects and strategies for effective professional development in nursing:
1. Continuous Learning:
Education and Training: Attend workshops, conferences, and seminars to stay updated on the latest advancements in healthcare.
Pursue additional certifications or advanced degrees to expand knowledge and expertise.
2. Specialization and Certification:
Specialization: Consider specializing in a particular area of nursing, such as critical care, pediatrics, or oncology.
Certification: Obtain relevant certifications to validate specialized skills and demonstrate commitment to professional excellence.
3. Clinical Experience:
Diverse Clinical Exposure: Seek diverse clinical experiences to broaden skills and understanding across different patient populations and healthcare settings.
4. Mentorship:
Establish Mentorship Relationships: Seek mentorship from experienced nurses or nursing leaders to gain insights, guidance, and advice in navigating your career.
Consider becoming a mentor to support the development of less experienced colleagues.
5. Professional Networking:
Professional Organizations: Join nursing associations and organizations to connect with peers, attend networking events, and access resources.
Online Platforms: Engage in online forums and social media groups to stay connected with the nursing community and share experiences.
6. Leadership Development:
Leadership Courses: Participate in leadership development programs or courses to enhance skills in management, decision-making, and team collaboration.
Leadership Roles: Take on leadership roles within your organization or professional associations to gain valuable leadership experience.
7. Research and Evidence-Based Practice:
Stay Informed: Stay updated on current research and evidence-based practices relevant to your area of nursing. Consider participating in research projects or contributing to evidence-based practice initiatives.
8. Interdisciplinary Collaboration:
Collaborate with Other Healthcare Professionals: Engage in collaborative projects with professionals from other healthcare disciplines to broaden perspectives and enhance teamwork.
9. Reflective Practice:
Self-Reflection: Regularly reflect on your nursing practice, identifying strengths, areas for improvement, and setting goals for professional growth.
Seek constructive feedback from peers and supervisors to inform your reflective practice.
10. Technology Integration:
Digital Literacy: Enhance digital literacy skills to effectively use technology in nursing practice. Stay informed about advancements in healthcare technology and incorporate relevant tools into your workflow.
11. Workshops and Seminars:
Participate Actively: Attend workshops and seminars on topics relevant to nursing practice, leadership, and personal development. Engage actively in discussions, share experiences, and learn from other participants.
12. Goal Setting:
Personal and Professional Goals: Set short-term and long-term goals for personal and professional development. Regularly revisit and adjust goals based on evolving career aspirations and industry changes.
Conclusion: Effective professional development is a dynamic and ongoing process that contributes to the growth and success of nurses throughout their careers. By embracing a commitment to continuous learning, seeking diverse experiences, and staying connected with the nursing community, nurses can enhance their skills, advance their careers, and make meaningful contributions to patient care.
| CHAPTER SIXCOMPASSIONATE AND PATIENT CARE |
COMPASSIONATE AND PATIENT CARE
Compassionate patient care is a cornerstone of nursing practice, emphasizing empathy, understanding, and a patient-centered approach. Here are key elements and strategies for providing compassionate patient care:
1. Empathy:
Understanding the Patient’s Perspective: Take the time to listen actively and understand the patient’s feelings, concerns, and experiences. Demonstrate empathy by acknowledging emotions and validating the patient’s experiences.
2. Communication:
Clear and Open Communication: Communicate with patients in a clear and understandable manner, avoiding medical jargon. Encourage questions and actively involve patients in their care decisions.
3. Respect and Dignity:
Respectful Interactions: Treat each patient with respect, recognizing their individuality and cultural background. Ensure privacy and maintain dignity during all aspects of care.
4. Active Listening:
Engaging in Active Listening: Practice active listening by giving full attention, making eye contact, and providing verbal and nonverbal cues that show attentiveness. Confirm understanding by summarizing or repeating information shared by the patient.
5. Personalized Care:
Individualized Care Plans: Develop care plans that are tailored to the unique needs, preferences, and values of each patient. Consider cultural, spiritual, and personal factors in providing personalized care.
6. Emotional Support:
Being Emotionally Present: Offer emotional support by being present, expressing genuine concern, and providing comfort during challenging times. Recognize and address emotional needs as an integral part of patient care.
7. Compassionate Touch:
Appropriate Physical Contact: Use compassionate touch when appropriate, such as holding a patient’s hand or offering a reassuring gesture. Ensure sensitivity to cultural and individual preferences regarding physical contact.
8. Cultural Competence:
Understanding Cultural Influences: Be aware of cultural differences and how they may impact a patient’s perceptions of care. Respect diverse cultural beliefs and practices in the provision of care.
9. Advocacy:
Patient Advocacy: Advocate for the patient’s rights, ensuring that their preferences and concerns are communicated and respected. Address any barriers to care and actively work to meet the patient’s needs.
10. Continuity of Care:
Consistent and Coordinated Care: Ensure continuity of care by coordinating with the healthcare team and providing consistent, reliable support. Communicate effectively during transitions of care to maintain a seamless patient experience.
11. Professional Boundaries:
Maintaining Professionalism: Establish clear professional boundaries while maintaining a compassionate and caring demeanor. Demonstrate empathy without over-identifying with patients to ensure objectivity.
12. Reflective Practice:
Continuous Self-Reflection: Engage in regular self-reflection to assess your own communication style, attitudes, and behaviors. Seek feedback from peers or mentors to enhance your capacity for compassionate care.
Conclusion: Compassionate patient care is an ongoing commitment that requires a combination of interpersonal skills, cultural sensitivity, and a patient-centered mindset. By integrating these elements into nursing practice, healthcare professionals can create a supportive and empathetic environment that contributes to positive patient experiences and outcomes.






You must be logged in to post a comment.